Introduction: The Frontline of Defense
It was a brisk morning when Nurse Jenny arrived at the long-term care facility, her mind preoccupied with the challenges of the day. The facility had recently admitted several new residents, and with flu season in full swing, Jenny knew that infection control would be more critical than ever. As she put on her scrubs and prepared for her shift, she couldn’t help but recall a conversation she had with her mentor, Nurse Evelyn, who had once told her, “Infection control isn’t just a set of rules—it’s a mindset, a commitment to protecting those in our care.”
Jenny had learned the hard way how essential infection control was. Early in her career, she had witnessed an outbreak of norovirus in a facility where she worked. It had spread rapidly, affecting both residents and staff. The experience left a lasting impression on her, making her realize that even small lapses in infection control practices could have devastating consequences. Today, Jenny was determined to ensure that every caregiver under her supervision understood the importance of infection control and adhered to best practices.
The Foundation: Hand Hygiene
One of the first lessons Jenny had learned about infection control was the critical importance of hand hygiene. It was a simple practice, but its impact on preventing the spread of infections could not be overstated. She remembered the words of her nursing school professor, who often said, “Your hands are your tools, but they can also be the biggest threat to your patients if not kept clean.”
Jenny had a routine she followed religiously: washing her hands thoroughly with soap and water before and after every patient interaction. She made sure to scrub for at least 20 seconds, paying close attention to areas like under the nails and between the fingers. When soap and water weren’t available, she used an alcohol-based hand sanitizer with at least 60% alcohol content.
But Jenny knew that it wasn’t enough for her to practice good hand hygiene—she needed to ensure that her colleagues did the same. She often found herself gently reminding others to wash their hands, especially during busy shifts when it was easy to overlook this crucial step. Jenny also educated new caregivers on the facility’s hand hygiene protocols, emphasizing that proper hand hygiene was the first line of defense against infections.
One day, Jenny noticed a new caregiver, Mark, who seemed to be in a hurry, neglecting to wash his hands between resident visits. She pulled him aside, not to scold him, but to share her own experience of the norovirus outbreak. “I know it seems like a small thing,” she told him, “but those few seconds can make all the difference in keeping our residents safe.” Mark appreciated the gentle reminder and soon became as vigilant about hand hygiene as Jenny was.
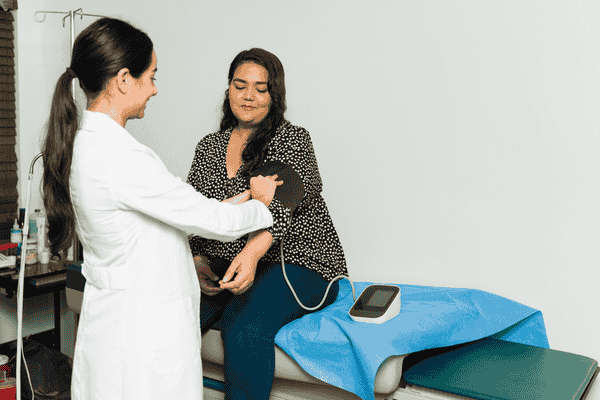
Personal Protective Equipment (PPE): A Shield Against Infection
As the COVID-19 pandemic swept across the globe, the use of personal protective equipment (PPE) became more prominent than ever. Jenny vividly remembered the early days of the pandemic when PPE shortages made it difficult for caregivers to feel safe while doing their jobs. The facility had implemented strict protocols on PPE use, and Jenny was tasked with ensuring that everyone adhered to them.
PPE was more than just gloves and masks—it was a crucial barrier between caregivers and potential infections. Jenny had always been diligent about wearing gloves when handling bodily fluids or performing procedures that could expose her to pathogens. However, the pandemic had introduced new practices, such as wearing masks at all times, using face shields, and donning gowns when entering certain areas of the facility.
Jenny recalled the anxiety that many caregivers felt during those early months. PPE was in short supply, and everyone had to be careful not to waste it. Jenny took it upon herself to teach her colleagues the proper way to don and doff PPE, emphasizing that improper removal could lead to contamination. She demonstrated how to remove gloves without touching the outside and how to carefully take off a mask without letting it touch their face.
One of the caregivers, Maria, expressed her concerns about feeling suffocated while wearing a mask for long hours. Jenny understood her discomfort but reminded her of the importance of protecting both themselves and the residents. “Think of the mask as your shield,” she said. “It’s not just for you—it’s for everyone around you.”
Over time, the caregivers grew more accustomed to the new normal. They developed a routine, ensuring that they always had the necessary PPE on hand and knew how to use it correctly. Jenny was proud of how her team had adapted, and she knew that their commitment to proper PPE use was a key factor in keeping the facility safe.
Environmental Cleaning: Maintaining a Safe Space
Jenny knew that infection control wasn’t just about what caregivers did—it was also about the environment in which they worked. Environmental cleaning played a critical role in preventing the spread of infections, and Jenny was meticulous about ensuring that the facility was kept clean and sanitized.
She often worked closely with the housekeeping staff, who were responsible for cleaning high-touch surfaces like doorknobs, handrails, and light switches. Jenny made sure they understood the importance of using the right disinfectants and following the correct procedures. She also encouraged the caregivers to take responsibility for cleaning equipment and supplies after each use.
Jenny remembered an incident from a few years back when an outbreak of Clostridioides difficile (C. diff) had occurred in the facility. C. diff is a bacterium that can cause severe diarrhea and colitis, and it spreads easily in healthcare settings. The outbreak had been traced back to inadequate cleaning practices, and Jenny was determined not to let that happen again.
She implemented a more rigorous cleaning protocol, ensuring that all surfaces were disinfected regularly and that proper cleaning agents were used. Jenny also made sure that the caregivers understood the importance of environmental cleaning and encouraged them to report any concerns about cleanliness in the facility.
One day, Jenny noticed that a resident’s bedside table had not been cleaned properly. She immediately alerted the housekeeping staff and took the opportunity to explain to the caregivers why it was so important to keep all surfaces clean. “Infections don’t just spread from person to person,” she said. “They can also spread from surfaces to people. We have to be vigilant in keeping our environment clean.”
The housekeeping staff appreciated Jenny’s dedication to infection control, and they worked together to maintain a safe and clean environment for the residents. Jenny knew that their efforts were paying off when the facility saw a significant decrease in infection rates.
Education and Training: Empowering Caregivers
Jenny understood that infection control was an ongoing process and that education and training were key to ensuring that caregivers had the knowledge and skills they needed to protect themselves and their residents. She regularly conducted training sessions on infection control practices, covering topics like hand hygiene, PPE use, and environmental cleaning.
One of Jenny’s most memorable training sessions was with a group of new caregivers who had just joined the facility. She began the session by sharing her personal experiences with infection outbreaks, including the norovirus and C. diff incidents. “I’ve seen firsthand what happens when we don’t take infection control seriously,” she said. “But I’ve also seen the difference we can make when we do.”
Jenny used a combination of lectures, demonstrations, and hands-on practice to ensure that the caregivers fully understood the infection control protocols. She encouraged them to ask questions and share their concerns, creating an open and supportive learning environment.
During the session, one of the new caregivers, Alex, expressed his nervousness about dealing with infectious diseases. Jenny reassured him that feeling anxious was normal, but emphasized that knowledge and preparation were the best ways to combat those fears. “The more you know, the more confident you’ll feel,” she said. “And remember, you’re not alone—we’re all in this together.”
By the end of the training, Jenny could see that the caregivers were more confident and prepared to take on the challenges of infection control. She reminded them that infection control wasn’t just about following protocols—it was about being proactive, staying informed, and always putting the safety of their residents first.
Conclusion: A Commitment to Safety
As Jenny reflected on her day, she felt a deep sense of pride in the work she and her colleagues were doing. Infection control was more than just a set of best practices—it was a commitment to the safety and well-being of the residents they cared for. Jenny knew that the efforts of every caregiver, from washing hands to wearing PPE to keeping the environment clean, played a crucial role in preventing infections.
Jenny’s journey as a nurse had taught her that infection control was a continuous process, one that required vigilance, dedication, and teamwork. As she walked through the facility, checking on residents and speaking with her colleagues, she was reminded of Nurse Evelyn’s words: “Infection control isn’t just a mindset—it’s a way of life.”
For Jenny and her team, mastering infection control was not just about following protocols—it was about embracing their role as protectors of those who trusted them with their care. And in that role, they found purpose, pride, and the knowledge that they were making a difference every day.