Are you a caregiver feeling overwhelmed by the responsibility of ensuring top-notch patient care? You’re not alone. In this comprehensive guide, we’ll explore 15 essential strategies that will transform your caregiving approach and elevate the quality and safety of your patient care.
From mastering clear communication with healthcare professionals to implementing fall prevention techniques, we’ve got you covered. We’ll delve into crucial aspects like:
• Effective medication management
• Creating a safe environment
• Providing emotional support
• Advocating for your patients
Whether you’re a family member caring for a loved one or a professional caregiver, these strategies will empower you to deliver compassionate, efficient, and safe care. Let’s embark on this journey to enhance your caregiving skills and make a lasting positive impact on your patients’ lives.
Importance of Clear Communication in Caregiving
Effective communication is the cornerstone of quality caregiving. It’s like the glue that holds everything together in the healthcare world.
Imagine trying to build a house without talking to your team. Chaos, right? The same goes for caregiving.
Good communication with healthcare professionals is crucial. It ensures everyone’s on the same page about the patient’s needs and treatment plan.
For example, let’s say your patient has a new medication. Clear communication with the doctor helps you understand:
– The correct dosage
– Potential side effects
– When to take it
– Any food interactions
This knowledge is vital for the patient’s safety and well-being.
But it’s not just about talking to doctors. Communication with the patient is equally important.
Think about it. How would you feel if someone was caring for you but never explained what they were doing? Pretty scary, right?
That’s why it’s essential to:
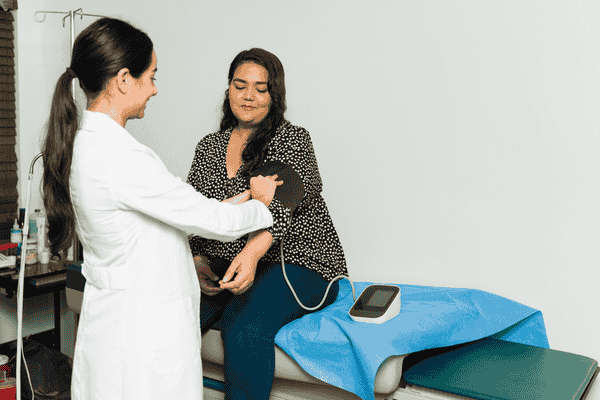
Explain Procedures Clearly
Before doing anything, tell the patient what you’re going to do. For instance:
“Mrs. Johnson, I’m going to check your blood pressure now. You’ll feel a slight squeeze on your arm, but it won’t hurt.”
This simple explanation can reduce anxiety and build trust.
Listen Actively
Communication is a two-way street. Pay attention to what the patient is saying – and not saying.
Are they wincing when they move? Are they avoiding certain topics? These non-verbal cues can provide valuable information about their condition.
Use Simple Language
Medical jargon can be confusing. Break it down into simple terms.
Instead of saying, “The patient is experiencing dyspnea,” say, “Mrs. Johnson is having trouble breathing.”
Communicate with Family Members
Family members are often an integral part of the care team. Keep them informed about:
– The patient’s progress
– Any changes in treatment
– How they can help
Clear communication with the healthcare team is also vital. It ensures continuity of care and prevents errors.
For instance, during shift changes, provide a detailed handover. This might include:
– The patient’s current condition
– Any medications given
– Upcoming tests or procedures
Remember, in caregiving, no detail is too small to communicate.
💡 Key Takeaways: Clear communication with healthcare professionals, patients, and families is crucial for ensuring safe, effective, and compassionate patient care.
Effective Medication Management for Patient Safety
Medication management is like being a superhero for your patient. You’re their first line of defense against medication errors and adverse events.
Think about it. One small mistake in medication can lead to big problems. It’s like putting diesel in a petrol car – it just doesn’t work!
Here’s how you can be a medication management superhero:
Know Your Medications
Understanding each medication is crucial. This includes:
– What it’s for
– How it should be taken
– Potential side effects
For example, if you’re giving a blood thinner, you need to know it increases the risk of bleeding. This knowledge helps you monitor the patient more effectively.
Double-Check Everything
Always verify the “five rights” of medication administration:
1. Right patient
2. Right drug
3. Right dose
4. Right route
5. Right time
Imagine giving Mrs. Smith’s heart medication to Mr. Jones. Yikes! That’s why double-checking is so important.
Keep Accurate Records
Document every medication given. It’s like keeping a diary for your patient’s health.
This record helps track:
– When medications were given
– Any reactions or side effects
– Changes in dosage
Understand Interactions
Some medications don’t play well together. It’s like putting a cat and a dog in the same room – sometimes it’s fine, sometimes it’s not.
For instance, certain antibiotics can decrease the effectiveness of birth control pills. Knowing these interactions can prevent increased risk to the patient.
Educate the Patient
Help the patient understand their medications. This might include:
– Why they’re taking it
– How to take it correctly
– What side effects to watch for
Remember, an informed patient is a safer patient.
Monitoring and Reporting Side Effects
Side effects can sneak up on you. It’s your job to be on the lookout.
For example, if a patient on blood pressure medication suddenly feels dizzy, it could be a side effect. Report this to the healthcare provider immediately.
Keep a close eye on:
– New symptoms
– Changes in behavior
– Unexpected reactions
Don’t hesitate to speak up if something seems off. You’re the patient’s advocate in their medical treatment.
Remember, effective medication management is a key part of healthcare practice. It’s not just about giving pills – it’s about ensuring the best possible outcome for your patient.
💡 Key Takeaways: Effective medication management involves thorough knowledge of medications, careful administration, accurate record-keeping, and vigilant monitoring for side effects to ensure patient safety and prevent adverse events.
Creating a Safe Environment: Fall Prevention Strategies
Falls are like uninvited guests at a party – they’re not welcome and can ruin everything. As a caregiver, your job is to be the bouncer, keeping falls out of your patient’s life.
Think about it. A fall can turn a simple hospital stay into a complicated ordeal. It’s like knocking over the first domino in a long line – one fall can lead to a cascade of health issues.
So, how do we create a fall-proof environment? Let’s dive in:
Assess the Risk
First, put on your detective hat. Look for clues that might increase fall risk:
– Physical limitations (like weak legs or poor eyesight)
– Medications that cause dizziness
– A history of falls
For example, if Mrs. Johnson takes blood pressure medication that makes her dizzy, she’s at higher risk for falls.
Clear the Path
Imagine trying to navigate an obstacle course blindfolded. That’s how some patients feel moving around their room.
Remove tripping hazards like:
– Loose rugs
– Clutter on the floor
– Tangled cords
Keep pathways clear and well-lit. It’s like creating a runway for safe movement.
Provide Support
Sometimes, patients need a helping hand – literally. Consider:
– Installing grab bars in bathrooms
– Using bed rails
– Providing walkers or canes
These tools are like training wheels on a bike – they provide extra stability and confidence.
Encourage Safe Footwear
Slippery socks on smooth floors? That’s a recipe for disaster.
Ensure patients wear:
– Non-slip socks or shoes
– Properly fitting footwear
– Nothing too loose or floppy
Think of it as giving your patient superhero boots – they provide grip and stability for safer movement.
Implement Safety Improvement Initiatives
Don’t be afraid to think big. Implement facility-wide strategies like:
– Regular staff training on fall prevention
– Using bed alarms for high-risk patients
– Conducting safety rounds to identify potential hazards
These initiatives are like setting up a safety net – they catch what individual efforts might miss.
Remember, creating a safe environment is an ongoing process. It’s not a one-and-done deal. Keep assessing, adapting, and improving your strategies.
Your efforts in fall prevention are crucial. You’re not just preventing injuries – you’re preserving your patient’s independence and quality of life.
💡 Key Takeaways: Creating a safe environment for patients involves assessing fall risks, clearing pathways, providing support tools, ensuring safe footwear, and implementing ongoing safety improvement initiatives to prevent falls and maintain patient safety.
Infection Control Practices for Caregivers
Think of infection control as your invisible shield. It protects both you and your patients from harmful germs. As a healthcare worker, you’re on the frontline of this battle against infections.
Imagine you’re a knight, and germs are the dragons. Your weapons? Soap, sanitizer, and smart practices!
Let’s break it down:
Hand Hygiene: Your First Line of Defense
Wash your hands like you’re about to perform surgery – because in a way, you are! Every time you touch a patient, you’re performing a delicate operation in infection control.
When should you wash? Follow the “5 Moments for Hand Hygiene”:
1. Before touching a patient
2. Before clean/aseptic procedures
3. After body fluid exposure risk
4. After touching a patient
5. After touching patient surroundings
Remember, alcohol-based hand sanitizers are your quick-draw weapon against germs. Use them often!
Personal Protective Equipment (PPE): Your Armor
Gloves, gowns, masks – these aren’t just fashion statements. They’re your armor in the fight against infections.
For example, when changing a wound dressing:
1. Put on gloves
2. Remove old dressing
3. Dispose of gloves
4. Wash hands
5. Put on new gloves
6. Apply new dressing
It’s like changing your shield between battles – each new task gets fresh protection.
Keep the Environment Clean
A clean environment is like a fortress against germs. In an efficient healthcare facility:
– Regularly disinfect high-touch surfaces (bed rails, doorknobs, light switches)
– Properly dispose of medical waste
– Follow protocols for handling soiled linens
Think of it as maintaining your castle – a clean space is a safe space.
Respiratory Hygiene
Teach patients the vampire cough – coughing into their elbow, not their hands. It’s like containing a sneeze bomb!
Provide tissues and hand sanitizer. Encourage their use. It’s a simple way to stop the spread of respiratory infections.
Remember, in infection control, you’re not just protecting one patient – you’re safeguarding the entire healthcare community. Your diligence can prevent outbreaks and save lives.
Stay vigilant, stay clean, and keep those germs at bay!
💡 Key Takeaways: Effective infection control for caregivers involves rigorous hand hygiene, proper use of personal protective equipment, maintaining a clean environment, and practicing good respiratory hygiene to create an efficient healthcare facility and prevent the spread of infections.
Ensuring Proper Nutrition and Hydration
Nutrition and hydration are the fuel that keeps our patients going. Think of the human body as a car – without the right fuel and enough water in the radiator, it just won’t run properly.
As a caregiver, you’re like the pit crew in a race, making sure your patient has everything they need to keep going.
Here’s how to ensure your patient stays well-nourished and hydrated:
Assess Nutritional Needs
Every patient is unique. A one-size-fits-all approach doesn’t work here. Consider:
– Age
– Weight
– Level of activity
– Chronic illnesses
For example, a patient with diabetes will have different nutritional needs than someone recovering from surgery.
Plan Balanced Meals
Create a meal plan that includes:
– Proteins (for muscle health)
– Carbohydrates (for energy)
– Fruits and vegetables (for vitamins and minerals)
– Healthy fats (for nutrient absorption)
It’s like creating a perfect recipe – all ingredients must be in the right proportion.
Monitor Fluid Intake
Dehydration can sneak up on patients, especially the elderly. Keep track of:
– How much they’re drinking
– Signs of dehydration (dry mouth, dark urine, dizziness)
Encourage regular fluid intake. It’s like keeping the car’s radiator full – it prevents overheating.
Accommodate Special Diets
Some patients may have dietary restrictions due to:
– Religious beliefs
– Food allergies
– Medical conditions
Respect these needs. It’s part of providing compassionate, personalized care.
Make Mealtime Pleasant
A pleasant eating environment can improve appetite. Consider:
– Sitting the patient up comfortably
– Providing assistance if needed
– Making the food look appealing
Remember, good nutrition isn’t just about the food – it’s about the whole eating experience.
By ensuring proper nutrition and hydration, you’re providing a high level of care that supports your patient’s overall health and recovery.
💡 Key Takeaways: Ensuring proper nutrition and hydration involves assessing individual needs, planning balanced meals, monitoring fluid intake, accommodating special diets, and creating a pleasant eating environment to support the patient’s overall health and recovery.
Providing Emotional Support to Care Recipients
As a caregiver, you’re not just tending to physical needs – you’re also a pillar of emotional support. Think of yourself as a lighthouse, guiding your care recipients through the stormy seas of their health challenges.
Emotional support is like a warm blanket on a cold day. It provides comfort, security, and helps your care recipients face their challenges with more courage.
Here’s how you can be that emotional anchor:
Practice Active Listening
Listening isn’t just hearing words. It’s about understanding the emotions behind them. When a family member or care recipient speaks:
– Give them your full attention
– Maintain eye contact
– Nod to show you’re following
For example, if Mrs. Johnson says, “I’m tired of all these tests,” she might really be saying, “I’m scared and overwhelmed.”
Show Empathy
Put yourself in their shoes. Imagine how you’d feel in their situation. Respond with compassion:
– “That must be really difficult for you.”
– “I can understand why you feel that way.”
It’s like building a bridge between you and your care recipient – empathy helps you connect on a deeper level.
Encourage Expression of Feelings
Create a safe space for care recipients to express themselves. Let them know it’s okay to feel scared, angry, or frustrated. You might say:
– “How are you feeling about your treatment?”
– “It’s okay to be upset. Would you like to talk about it?”
Think of it as opening a pressure valve – allowing emotions out can relieve stress and anxiety.
Offer Reassurance
Sometimes, a little reassurance goes a long way. It’s like offering a life vest in choppy waters. You might say:
– “We’re here to support you every step of the way.”
– “You’re doing great. It’s normal to have ups and downs.”
Respect Privacy and Dignity
Remember, your care recipients are individuals with their own thoughts and feelings. Respect their privacy and maintain their dignity. This might mean:
– Knocking before entering their room
– Asking permission before performing care tasks
– Covering them appropriately during procedures
It’s about treating them as you would want to be treated – with respect and consideration.
Use Touch Appropriately
A gentle touch on the arm or shoulder can convey support and comfort. But always ask first – some people may not be comfortable with physical contact.
Celebrate Small Victories
Acknowledge and celebrate progress, no matter how small. It could be:
– Taking a few steps after surgery
– Eating a full meal
– Having a good night’s sleep
These celebrations are like planting seeds of positivity – they can grow into improved mood and outlook.
Remember, providing emotional support is a crucial part of compassionate patient care. It can make a world of difference in your care recipient’s experience and overall well-being.
💡 Key Takeaways: Providing emotional support to care recipients involves active listening, showing empathy, encouraging expression of feelings, offering reassurance, respecting privacy and dignity, using appropriate touch, and celebrating small victories to enhance the overall care experience.
Advocating for Patients in the Healthcare System
As a caregiver, you’re not just a helper – you’re a champion for your patients. Think of yourself as their personal superhero, navigating the complex world of healthcare on their behalf.
Advocacy is like being a GPS in the healthcare maze. You help patients find the best route to quality care and ensure their voice is heard.
Here’s how you can be a powerful advocate:
Know the Patient’s Rights
Understanding patient rights is like knowing the rules of the game. It helps you play better. These rights typically include:
– The right to information about their condition
– The right to make decisions about their care
– The right to privacy and confidentiality
For example, if a doctor suggests a treatment without explaining alternatives, you can step in and ask for more information on behalf of your patient.
Be the Voice
Sometimes, patients feel intimidated or overwhelmed in medical settings. That’s where you come in. Speak up when they can’t. For instance:
– If a patient is in pain but hesitant to ask for medication
– If they don’t understand a doctor’s explanation
– If they have concerns about their treatment plan
It’s like being their translator in the language of healthcare.
Ask Questions
Don’t be afraid to ask questions. It’s not about challenging authority – it’s about ensuring the best care. Some key questions might be:
– “What are the potential side effects of this treatment?”
– “Are there alternative options we should consider?”
– “How will this affect the patient’s daily life?”
Think of it as being a detective – gathering all the clues to solve the case of your patient’s best care.
Coordinate Care
In today’s healthcare system, patients often see multiple specialists. You can play an active role in coordinating this care. This might involve:
– Keeping track of appointments
– Ensuring different doctors are aware of all medications
– Sharing important information between healthcare providers
It’s like being the conductor of an orchestra – making sure all parts work together harmoniously.
Encourage Patient Involvement
While you’re their advocate, remember to involve the patient in their own care. Encourage them to:
– Ask questions
– Express their preferences
– Make informed decisions
It’s about empowering them to be active participants in their health journey.
Stay Informed
Keep up-to-date with the latest in healthcare. This might mean:
– Researching the patient’s condition
– Understanding new treatment options
– Knowing about relevant clinical trials
Think of it as sharpening your tools – the more you know, the better you can advocate.
Document Everything
Keep detailed records of:
– Symptoms
– Medications
Conclusion
As we conclude this comprehensive guide on essential strategies for caregivers, it’s clear that providing high-quality, safe patient care is both an art and a science. By implementing these 15 strategies, from effective communication to holistic care approaches, caregivers can significantly enhance the well-being of their care recipients. Remember, your role as a caregiver is invaluable, and your dedication makes a profound difference in the lives of those you care for.
We encourage you to continuously refine your skills, prioritize self-care, and stay connected with healthcare professionals and community resources. By doing so, you’ll not only improve patient outcomes but also find greater fulfillment in your caregiving journey. Thank you for your commitment to compassionate patient care. As you move forward, may you feel empowered to provide the best possible care, knowing that your efforts contribute to a higher quality of life for your care recipients.