Have you ever stopped to ponder the intricate ways in which strokes can manifest themselves in aging individuals? Picture this – subtle changes in behavior, unexplained fatigue, or sudden bouts of confusion. These can all be telltale signs of stroke, a condition where time is of the essence. In the realm of aging individuals, strokes can present themselves in unusual and unexpected ways, often masking their true nature amidst the complexities of the aging process.
As we delve deeper into the rare and atypical symptoms of stroke in older adults, we’ll unravel a web of intricacies that challenge conventional diagnostic norms. From the depletion of senescent cells to the role of mitochondrial dysfunction, we’ll navigate through the maze of aging-related diseases that can cloud the stroke diagnosis landscape. Armed with insights into the nuances of stroke presentations in the aging population, we aim to shed light on the complexities that healthcare professionals face when identifying and managing these unique cases.
Introduction to Atypical Stroke Presentations
Stroke, a leading cause of disability and mortality, commonly presents with well-known focal neurological deficits such as weakness, speech difficulties, and sensory loss. However, in aging individuals, stroke can exhibit unusual and rare symptoms that warrant attention and a deeper understanding.
In this article, we explore the nuances of atypical stroke presentations in the elderly population. It is crucial to recognize that these manifestations may differ from the classic symptoms seen in younger individuals, leading to potential diagnostic challenges.
Understanding the diverse range of stroke presentations is essential for healthcare professionals and researchers involved in stroke management and prevention. By recognizing and addressing atypical symptoms promptly, it is possible to improve patient outcomes and minimize potential disabilities.
While traditional focal neurological deficits are still prevalent in older adults, there are intriguing cases where stroke manifests in unexpected ways. By exploring these uncommon presentations, we hope to shed light on the subtle signs that may indicate stroke in aging individuals.
Non-localizing Symptoms in Stroke
When it comes to stroke, the image that often comes to mind is that of a sudden loss of strength or sensation on one side of the body, accompanied by difficulty speaking or understanding. However, it is important to recognize that stroke presentations can vary significantly, especially in aging individuals. These non-localizing symptoms can be quite perplexing, as they do not follow the traditional pattern of focal neurological deficits. Let’s explore some of these atypical manifestations of stroke in older adults.
Cognitive and Behavioral Changes
Meet Mary, an energetic grandmother of six who loves spending her weekends baking cookies and gardening. One sunny afternoon, while tending to her roses, Mary suddenly felt a sharp pain in her head, her vision blurred, and she found herself unable to move her right arm. It was a terrifying moment that changed her life in an instant. Mary had suffered a stroke.
Mary’s story highlights how strokes in older adults can sometimes present with cognitive and behavioral changes. Some aging individuals may experience sudden cognitive impairments or confusion, which can be signs of a stroke. It is crucial to consider stroke as a potential cause, especially when these changes occur suddenly and without a clear explanation. Additionally, mood disturbances such as depression, anxiety, and changes in personality can sometimes be the first indicators of a stroke in older adults. These non-localizing emotional symptoms can easily be misinterpreted or attributed to other factors, resulting in delayed diagnosis.
Vestibular Symptoms
- Dizziness and vertigo: While dizziness is a common complaint among older adults, it can also be a manifestation of a stroke. Vertigo, a spinning sensation, can occur when there is a disruption in blood flow to the brain. It is essential to investigate the possibility of stroke when these symptoms are present.
Syncope and Falls
- Transient loss of consciousness (syncope): Older adults experiencing unexplained episodes of syncope should undergo a thorough evaluation, as this symptom can sometimes be associated with an underlying stroke. It is particularly important to consider stroke when syncope is accompanied by other neurological signs.
- Frequent falls: Falls are a significant concern in the aging population. While often attributed to age-related balance and coordination issues, recurrent falls can also be an indicator of an underlying stroke. Evaluation for stroke should be considered, especially when falls occur without an apparent cause.
Altered Sensations
- Tingling or numbness: Stroke can present as altered sensations in aging individuals. Tingling or numbness in the face, arms, or legs may occur without the characteristic one-sided weakness typically associated with stroke.
- Sensory disturbances: Unusual sensory changes, such as abnormal heat or cold sensations, can occur in strokes that affect sensory pathways. These non-localizing symptoms pose unique challenges for diagnosis.
It is important for healthcare professionals and caregivers to be aware of these non-localizing symptoms of stroke in aging individuals. Early recognition and prompt medical attention can significantly improve outcomes. When assessing older adults with these atypical manifestations, a comprehensive evaluation considering the possibility of stroke is crucial.
Remember, if you or someone you know is experiencing any of these symptoms, seek immediate medical attention. Stroke is a medical emergency, and timely intervention can prevent long-term disability and save lives.
Abnormal Movements or Seizures in Stroke
When it comes to stroke presentations, the common signs and symptoms often involve focal neurological deficits. However, there are instances where stroke can manifest in atypical ways, including abnormal movements and seizures. These unusual motor symptoms can present challenges for diagnosis and management in aging individuals.
Chorea and Hemichorea
Chorea and hemichorea are hyperkinetic movement disorders characterized by involuntary, purposeless movements. In the context of stroke, these abnormal movements can occur on one side of the body (hemichorea) or involve both sides (chorea). They often result from damage to the contralateral basal ganglia, primarily the caudate nucleus or putamen. These movement abnormalities can be subtle or pronounced, causing significant functional impairment.
Mary’s friend, John, an 80-year-old retired teacher, experienced such symptoms. John noticed involuntary movements in his left hand that seemed to dance on their own. Initially dismissing them as part of aging, he eventually consulted his doctor, who diagnosed him with stroke-induced hemichorea. Early intervention helped John manage his symptoms effectively, preventing further complications.
Seizures
Seizures can also be an atypical presentation of stroke in older adults. These can range from focal seizures, affecting a small part of the brain, to generalized seizures, impacting both hemispheres. Recognizing seizures as a possible manifestation of stroke is crucial for timely diagnosis and treatment.
In John’s case, his involuntary movements were accompanied by brief episodes of confusion, which were later identified as focal seizures. His neurologist emphasized the importance of understanding these unusual presentations, especially in older adults, to ensure appropriate and prompt treatment.
Peripheral Nervous System Involvement
Stroke is primarily associated with central nervous system involvement, but it can also affect the peripheral nervous system, leading to symptoms like neuropathy and muscle weakness.
Neuropathy
Peripheral neuropathy can manifest as a result of stroke, causing numbness, tingling, and pain in the extremities. These symptoms can be mistaken for other conditions like diabetic neuropathy or age-related nerve degeneration.
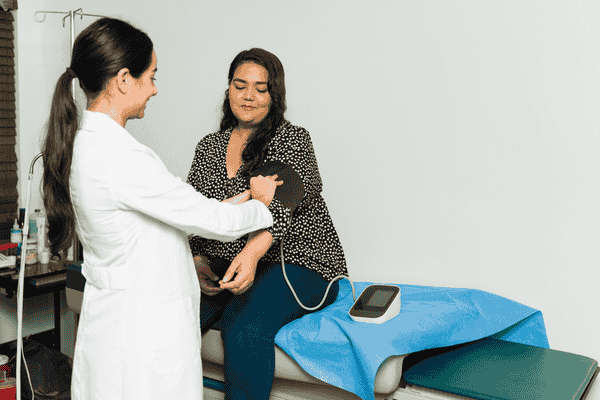
John’s neighbor, Susan, a vibrant 75-year-old artist, experienced persistent tingling and numbness in her feet and hands. Initially attributed to her diabetes, a comprehensive evaluation revealed that a mild stroke had contributed to her neuropathy. Understanding this connection helped Susan receive targeted treatment, improving her quality of life.
Conclusion: Recognizing the Unseen
The stories of Mary, John, and Susan highlight the diverse and atypical ways strokes can present in aging individuals. Recognizing these unusual symptoms is crucial for timely diagnosis and intervention. Healthcare professionals and caregivers must maintain a high index of suspicion and consider stroke as a potential cause, even when symptoms deviate from the classic presentations.
By understanding the breadth of stroke manifestations, we can improve outcomes and enhance the quality of care provided to aging individuals experiencing these unusual symptoms. If you or someone you know experiences any of these atypical signs, seek immediate medical attention. Early detection and treatment can make all the difference in managing stroke and its consequences.
Stay tuned as we continue to explore the fascinating world of stroke in aging individuals. Together, we can unravel the complexities and improve the lives of those affected by this condition.