It was a quiet afternoon at the clinic, and Dr. Sarah Montgomery was reviewing her notes when Mrs. Elaine Carter walked into her office. Mrs. Carter, an 82-year-old woman with a sharp wit and a warm smile, had been coming to the clinic for years. Over the past few months, however, there had been a change in her demeanor. She had become more reserved and, as Dr. Montgomery suspected, a bit embarrassed about something. Today, she had finally decided to open up about the urinary issue.
“Doctor,” Mrs. Carter began, her voice hesitant, “I’ve been having some trouble lately… with my bladder.”
Dr. Montgomery wasn’t surprised. Urinary incontinence is a common condition among elderly patients, and yet it is one of the most underreported due to the stigma and embarrassment that often accompanies it. She knew that addressing Mrs. Carter’s concerns with empathy and care was the first step toward helping her regain her confidence and independence.
As Dr. Montgomery prepared to conduct a thorough examination, she reflected on the key physical examination techniques she would use to evaluate Mrs. Carter’s condition. Urinary incontinence, after all, could have several causes, and understanding the root of the problem would allow for the most effective treatment plan. For other healthcare providers like her, mastering these techniques is crucial for offering the best care to elderly patients facing this sensitive issue.
1. Inspection and Palpation of the Abdomen
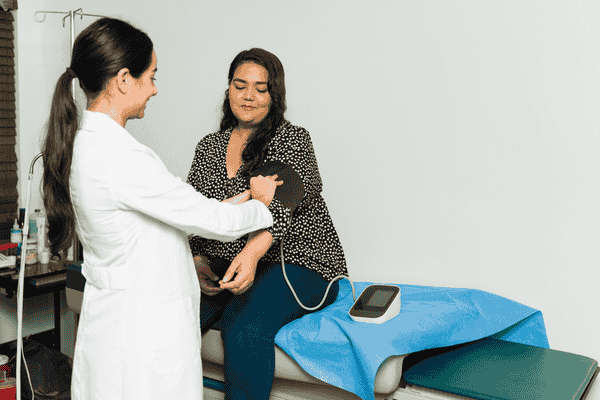
The first step in evaluating urinary incontinence is to perform an abdominal examination. Dr. Montgomery gently guided Mrs. Carter to lie down on the examination table, explaining what she would be doing every step of the way. She began with an inspection and palpation of the abdomen to assess for any distension, masses, or tenderness.
For elderly patients like Mrs. Carter, bladder distension can be a sign of urinary retention, which can sometimes be misinterpreted as incontinence. By carefully palpating the bladder area, Dr. Montgomery could determine if Mrs. Carter’s bladder was overly full, indicating a potential blockage or issue with emptying.
The inspection also allowed Dr. Montgomery to rule out other potential causes of Mrs. Carter’s symptoms, such as a hernia or other abdominal masses that could be pressing on the bladder and contributing to incontinence.
2. Pelvic Examination
After completing the abdominal examination, Dr. Montgomery explained that the next step would be a pelvic examination. Mrs. Carter, though a bit nervous, appreciated the doctor’s calm and gentle approach. Pelvic exams are particularly important for women experiencing urinary incontinence, as they allow the physician to assess the health of the pelvic organs and muscles.
Dr. Montgomery knew that pelvic floor weakness is a leading cause of stress urinary incontinence in elderly women. By examining the vaginal walls and pelvic muscles, she could determine if Mrs. Carter’s pelvic support structures had weakened over time, which is common after menopause. This weakness can lead to the bladder and urethra shifting out of place, causing leakage during activities that increase abdominal pressure, such as coughing, sneezing, or laughing.
Additionally, during the pelvic exam, Dr. Montgomery checked for signs of atrophic vaginitis, a condition that occurs in postmenopausal women due to decreased estrogen levels. This thinning and inflammation of the vaginal tissues can also contribute to incontinence by affecting the urethra.
3. Rectal Examination
While Mrs. Carter had expressed concern about her bladder, Dr. Montgomery knew that it was important to conduct a rectal examination as well. This examination could provide valuable information about Mrs. Carter’s overall pelvic health, particularly the function of the pelvic floor muscles.
By asking Mrs. Carter to perform a voluntary contraction of the pelvic floor muscles, Dr. Montgomery was able to assess the strength of these muscles, which play a critical role in maintaining continence. Weak pelvic floor muscles can contribute not only to urinary incontinence but also to fecal incontinence, a condition that often coexists in elderly patients.
The rectal exam also allowed Dr. Montgomery to check for the presence of fecal impaction. In some cases, severe constipation can lead to overflow incontinence, where the bladder becomes overly full and leaks urine due to pressure from impacted stool. This is especially common in elderly patients who may have slower bowel movements or difficulty with regular elimination.
4. Cough Stress Test
After completing the internal examinations, Dr. Montgomery moved on to a more functional assessment: the cough stress test. She explained to Mrs. Carter that she would be asked to cough forcefully while lying down and again while standing. This simple yet effective test helps evaluate the presence of stress urinary incontinence.
During the test, Dr. Montgomery observed whether urine leakage occurred when Mrs. Carter coughed. In cases of stress incontinence, the increased pressure in the abdomen during a cough or sneeze can cause urine to leak out, especially if the pelvic floor muscles are weak. This test provided Dr. Montgomery with real-time insight into how Mrs. Carter’s body responded to physical stressors.
The cough stress test is a quick and reliable way to confirm stress incontinence and can help guide further treatment options, such as pelvic floor muscle exercises or, in more severe cases, surgical interventions.
5. Post-Void Residual (PVR) Measurement
Dr. Montgomery knew that understanding how well Mrs. Carter’s bladder was emptying was a key part of the evaluation. After Mrs. Carter used the restroom, Dr. Montgomery used an ultrasound device to measure her post-void residual (PVR)—the amount of urine left in the bladder after urination.
In healthy individuals, the bladder should empty almost completely during each trip to the bathroom. However, for elderly patients, issues such as bladder outlet obstruction ou weak bladder muscles can prevent complete emptying, leading to urinary retention and, eventually, overflow incontinence.
By using a bladder scan or a catheterization procedure, Dr. Montgomery could determine if Mrs. Carter’s bladder was holding on to too much urine after voiding, which would indicate a potential problem with bladder function or a blockage in the urinary tract.
6. Neurological Examination
Finally, Dr. Montgomery conducted a brief neurological examination. This step was crucial in determining if Mrs. Carter’s incontinence might be related to an underlying neurological issue, such as spinal cord injury, multiple sclerosis, or Parkinson’s disease.
By assessing Mrs. Carter’s reflexes, muscle strength, and sensation in the lower body, Dr. Montgomery could rule out or identify any potential nerve damage that might be affecting her bladder control. For example, if the nerves that control the bladder are damaged, it can lead to urge incontinence, where the patient feels a sudden and intense need to urinate but is unable to hold it long enough to reach the bathroom.
In elderly patients, conditions such as diabetes et stroke can also lead to nerve damage that affects bladder function, making this neurological assessment an important part of the overall evaluation.
The Road to Recovery
After completing the series of physical examinations, Dr. Montgomery sat down with Mrs. Carter to discuss the findings. It was clear that Mrs. Carter’s urinary incontinence was a combination of stress incontinence, due to weakened pelvic floor muscles, and some urge incontinence, likely related to overactive bladder symptoms.
Dr. Montgomery assured Mrs. Carter that incontinence is a common and treatable condition. Together, they devised a plan that included pelvic floor muscle exercises, dietary adjustments, and medications to help control her symptoms. For Mrs. Carter, just knowing that there was a path forward was a relief.
As she left the clinic that day, Mrs. Carter felt a sense of hope. By opening up about her symptoms and undergoing a thorough physical examination, she had taken the first step toward regaining control over her bladder—and her life. Dr. Montgomery had not only diagnosed her condition but also empowered her to take charge of her health with confidence.
Conclusion: Comprehensive Physical Examinations for Elderly Incontinence
Evaluating urinary incontinence in the elderly requires a comprehensive approach, combining various physical examination methods to assess bladder function, pelvic floor strength, and neurological health. By mastering these essential techniques, healthcare providers can offer elderly patients like Mrs. Carter the best possible care, leading to improved quality of life and, most importantly, dignity.