Sarah watched her mother struggle with daily tasks, knowing something needed to change. After her mother’s recent diagnosis of early-stage Parkinson’s disease, the family faced countless decisions about her care. The endless medical appointments, medication schedules, and daily care needs seemed overwhelming until they worked with a dedicated care coordinator to develop a personalized care plan. “The difference was immediate,” Sarah recalls. “Instead of feeling overwhelmed, we had a clear roadmap for Mom’s care that considered not just her medical needs, but her whole life. It was like finally having a compass in what felt like an endless maze.”
In the intricate landscape of caregiving, meeting specific health needs stands as the cornerstone of providing quality care for our loved ones. Personalized care plans have emerged as a powerful tool, offering a structured yet flexible approach to addressing unique medical conditions, personal preferences, and daily routines. These carefully crafted plans represent a departure from traditional one-size-fits-all solutions, acknowledging that each individual’s journey through aging or illness is unique. By creating a comprehensive framework that adapts to changing needs while maintaining consistency in care delivery, personalized care plans have revolutionized how we approach long-term care and support for those who need it most.
Understanding Personalized Care Plans
What is a Personalized Care Plan?
A personalized care plan serves as more than just a document – it’s a dynamic, living roadmap that guides the delivery of individualized care while preserving dignity and autonomy. These plans emerge from a deep understanding that effective care must balance medical necessities with personal preferences, cultural values, and lifestyle choices. They represent a collaborative effort between healthcare providers, caregivers, family members, and most importantly, the individual receiving care, ensuring that every aspect of their well-being is considered and addressed.
Consider James, an 82-year-old retired teacher with diabetes and early cognitive decline. His care plan transcends basic medical management to encompass his entire life experience. The plan carefully integrates his daily medication schedule with his preferred routine of morning walks in the garden, acknowledging how this activity not only helps manage his blood sugar but also maintains his connection to nature – a passion he developed during his teaching years. His care plan includes modifications to his living space that support independence while ensuring safety, and it even incorporates his love for classical music during meals, which has been shown to improve his eating habits and overall mood. This comprehensive approach ensures that James receives care that honors both his medical needs and his identity as an individual, allowing him to maintain a sense of self even as his needs change.
The Evolution of Care Planning
The journey toward personalized care planning reflects a broader shift in healthcare philosophy, moving away from institutional, procedure-focused care toward a more holistic, person-centered approach. This evolution recognizes that effective care must consider the intricate interplay between physical health, emotional well-being, social connections, and environmental factors. Modern care plans have become increasingly sophisticated, incorporating evidence-based practices while remaining flexible enough to accommodate individual preferences and changing needs.
Essential Components of a Care Plan
A comprehensive care plan encompasses multiple interconnected elements that work together to support an individual’s overall well-being. At its foundation, the plan begins with detailed medical management protocols, but it extends far beyond basic healthcare to address every aspect of daily living and quality of life.
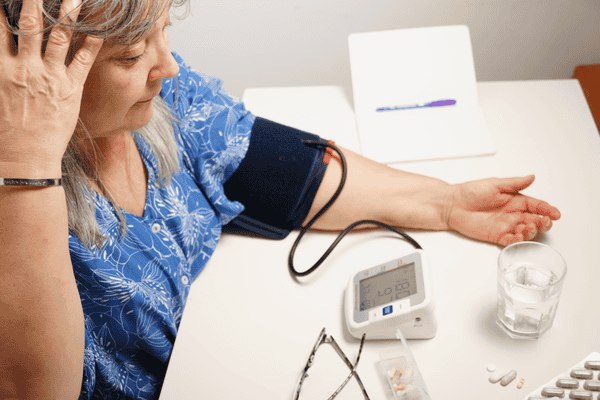
Medical Care and Health Monitoring
The medical component of a care plan includes comprehensive documentation of current health conditions, medication schedules, and specific treatment protocols. For instance, when Barbara, who lives with diabetes and arthritis, received her care plan, it included detailed instructions for insulin administration, blood sugar monitoring schedules, and specific guidance for managing arthritis flare-ups. The plan also incorporated regular vital sign monitoring, scheduling of routine medical appointments, and clear protocols for emergency situations.
Daily Living Support
Personal care assistance forms a crucial part of many care plans, detailing support needed with activities of daily living (ADLs). This encompasses morning and evening routines, bathing schedules, dressing assistance, and grooming preferences. The plan specifies not just what assistance is needed, but how it should be provided to maintain dignity and maximize independence. For example, Tom’s care plan includes step-by-step guidance for his morning routine, incorporating his preference for shaving before showering and allowing extra time for him to dress independently with minimal assistance.
Nutrition and Dietary Management
Nutritional planning goes beyond basic meal scheduling to include dietary restrictions, food preferences, and specific feeding assistance needs. A well-crafted nutritional plan considers texture modifications for swallowing difficulties, cultural food preferences, and timing of meals to coordinate with medication schedules. The plan might detail preferred snacks, hydration requirements, and strategies for encouraging adequate nutrition when appetite is poor.
Physical Activity and Exercise
Exercise and physical activity recommendations are tailored to individual capabilities and preferences. This might include structured physical therapy exercises, daily walking routines, or modified movement activities for those with limited mobility. The plan specifies safety precautions, recommended duration and frequency of activities, and signs that indicate when to modify or stop physical activity.
Social and Emotional Support
Care plans address psychological and social needs through scheduled activities, social interactions, and emotional support strategies. This might include arrangements for regular family visits, participation in community activities, or engagement in hobby groups. For those with cognitive decline, the plan might include memory care activities and communication strategies for caregivers.
Environmental Safety Measures
Home safety considerations are detailed in the care plan, including necessary home modifications, fall prevention strategies, and emergency response protocols. This might involve recommendations for installing grab bars, removing trip hazards, or implementing a medical alert system.
Special Care Instructions
Many care plans include specific instructions for managing unique medical devices or treatments, such as wound care protocols, catheter management, or oxygen therapy. These instructions provide detailed guidance for both professional caregivers and family members involved in care delivery.
Communication and Coordination
The plan outlines comprehensive communication protocols between all involved parties – healthcare providers, family members, and caregivers. A critical component is a clearly prioritized list of emergency contacts, including primary and secondary family contacts, the individual’s primary care physician, relevant specialists, and preferred emergency medical services. This emergency contact protocol typically includes detailed instructions for different scenarios – when to call family members versus when to contact medical professionals or emergency services. The plan also specifies which situations warrant calling his cardiologist directly versus going to the emergency room. Beyond emergency situations, the plan details how routine information should be shared, who should be contacted for various non-emergency situations, and how care transitions should be managed.
Medication Management
Beyond basic medication schedules, the plan includes detailed information about proper administration techniques, potential side effects to monitor, and strategies for ensuring medication compliance. It might also include protocols for pain management and PRN (as-needed) medications.
Quality of Life Considerations
Personal preferences and lifestyle choices are integrated throughout the care plan, ensuring that care delivery aligns with individual values and desires. This includes preferred daily routines, recreational activities, spiritual practices, and other elements that contribute to quality of life.
Each of these components is carefully tailored to individual needs and preferences, creating a holistic approach to care that promotes both physical health and emotional well-being. The plan addresses not just what care should be provided, but how it should be delivered in a way that respects the individual’s preferences and promotes their autonomy. For instance, rather than simply scheduling medication times, the plan might specify that certain medications work better when taken with particular meals, incorporating this into the individual’s natural daily rhythm rather than imposing a rigid schedule that disrupts their routine.
The Impact of Personalized Care
Transforming Health Outcomes
The implementation of personalized care plans has demonstrated remarkable success in improving health outcomes across various conditions and circumstances. Take Mary, a 75-year-old with congestive heart failure, whose experience illustrates the transformative power of personalized care. Prior to implementing her tailored care plan, Mary frequently visited the emergency room due to fluid retention and breathing difficulties. Her new care plan integrated daily weight monitoring, carefully planned sodium restriction, and a graduated exercise program specifically designed around her capabilities and interests. The result was a 60% reduction in hospital visits, but more importantly, Mary reported feeling more in control of her health and more confident in managing her condition.
These improvements stem from the plan’s ability to address not just the medical aspects of care but also the behavioral and environmental factors that influence health outcomes. By considering how an individual’s daily routines, living environment, and support systems impact their health, personalized care plans create a more sustainable approach to managing chronic conditions and maintaining overall wellness.
Emotional and Psychological Benefits
The psychological impact of personalized care extends far beyond medical outcomes, creating ripple effects that touch every aspect of an individual’s life. When people feel their preferences and values are respected, they experience a profound sense of dignity and self-worth that contributes to better mental health outcomes. This emotional well-being often translates into improved physical health, creating a positive feedback loop that enhances overall quality of life.
Through careful attention to personal preferences and the maintenance of meaningful activities, personalized care plans help individuals maintain their sense of identity and purpose even as they navigate health challenges. This preservation of personal identity has been shown to reduce rates of depression and anxiety among those receiving long-term care, while also improving their engagement with therapeutic activities and medical treatments.
Supporting Family Caregivers
The benefits of personalized care plans extend to family caregivers, who often struggle with the emotional and practical challenges of providing care. These plans offer clear guidelines and expectations, helping to reduce the uncertainty and stress that frequently accompany the caregiving journey. By providing a structured framework for care delivery while maintaining flexibility for adaptation, care plans help family members balance their caregiving responsibilities with their own lives and well-being.
Implementation and Evolution
Collaborative Development
The development of an effective care plan requires extensive collaboration between healthcare providers, caregivers, and the individual receiving care. This process begins with a comprehensive assessment that considers medical history, current health status, functional capabilities, cognitive status, and personal preferences. However, the true art of care planning lies in how this information is synthesized into a cohesive strategy that addresses both immediate needs and long-term goals.
Healthcare providers contribute their clinical expertise, while family members and caregivers offer invaluable insights into the individual’s daily routines, preferences, and challenges. The individual’s own goals and preferences serve as the cornerstone of the plan, ensuring that care remains focused on what matters most to them. This collaborative approach ensures that the resulting plan is both medically sound and practically implementable within the context of the individual’s life.
Adaptation and Refinement
Care plans must remain dynamic, evolving to meet changing needs and circumstances while maintaining consistency in core care principles. Regular reviews and updates ensure that the plan continues to serve its intended purpose effectively, with modifications made as needed to address new challenges or opportunities for improvement. This ongoing refinement process involves not just updating medical protocols but also reassessing how well the plan aligns with the individual’s current preferences and goals.
Looking Ahead: The Future of Personalized Care
As healthcare continues to evolve, personalized care plans are becoming increasingly sophisticated, incorporating new technologies and approaches while maintaining their fundamental focus on individual needs and preferences. Digital health monitoring tools now allow for more precise tracking of health metrics, while telehealth services expand access to specialized care and support. Artificial intelligence applications are beginning to assist in identifying patterns and predicting potential health issues, enabling more proactive care approaches.
However, the essence of personalized care remains firmly rooted in human connection and understanding. As Sarah discovered with her mother’s care, the right personalized care plan can transform the caregiving journey from one of stress and uncertainty to one of confidence and connection. “Now we don’t just manage Mom’s condition,” Sarah shares, “we help her live her best possible life. The care plan has given us a framework to ensure she receives the medical care she needs while still being able to enjoy the things that make her happy – her garden, her book club, and most importantly, her independence.”
Conclusion
Personalized care plans represent more than just a structured approach to caregiving – they embody a fundamental commitment to treating each individual with the dignity and respect they deserve. Through careful attention to both medical needs and personal preferences, these plans create a framework for care that enhances quality of life while promoting independence and well-being. As healthcare continues to evolve, the principles of personalized care planning will remain essential to providing compassionate, effective support for those who need it most.




My brother suggested I might like this blog. He was entirely right.
This post actually made my day. You can not imagine simply how much time I had spent
for this information! Thanks!